Introduction
“3D printing can use various materials (plastic, metal, ceramics, living cells) in layers to produce a 3D object. The object is built vertically layer by layer allowing creation of the complex structures” (Mikolajewska et al, 2014). “Organ printing or biomedical application of rapid prototyping, also defined as additive layer-by-layer biomanufacturing, is an emerging transforming technology that has potential for surpassing traditional solid scaffold-based tissue engineering” (Mironov et al, 2008). According to Mironov et al (2008), it is an automated approach that offers a pathway for scalable reproducible mass production of tissue engineered products; it allows a precise simultaneous 3D positioning of several cell types; it enables creation tissue with a high level of cell density; it can solve the problem of vascularization in thick tissue constructs; finally, organ printing can be done in situ. According to Griggs (2014), scientist harvests human cells from biopsies or stem cells then allowing them to multiply. This mixture is used as ink and is fed into the 3D printer which is programmed to re-arrange different cell types along with other materials into a precise 3D shape.The above description of 3D printing is specific to 3D printing of human organs.
“The ultimate goal of organ-printing technology is to fabricate 3D vascularized functional living human organs suitable for clinical implantation” (Mironov et al, 2008). According to Mironov et al (2008), there are five essential components, in order to print a living human organ, it is necessary to have a computer-aided design of the desired organ, a ‘bioprinter’ or robotic dispenser, a cartridge or container for dispensing biomaterials and living cells or cell aggregates, processible biomimetic hydrogel, and a self-assembling cell aggregates or single cells in hydrogels.
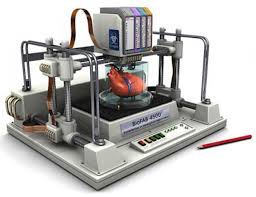
The above image is a 3d printer that prints organs.
The above images are examples of prosthetic limb made by a 3d printer.
CLINICAL IMPLICATIONS
As with any new technology, it’s easy to get swept up in the benefits of 3D printing. It opens up a world of new possibilities for all industries, and stands to lessen transportation costs, environmental impacts, waste, and reliance on corporations by enabling the maker movement. “Broader use of such technologies may cause developing customization/personalization of various medical products and lower cost of design and manufacturing” (Mikolajewska et al, 2014). According to Mikolajewska et al, 2014, a problem constitutes to the application of proper materials in particular cases – there is need for development of novel materials for 3D printing, dedicated to the medical applications (e.g. in anti-allergic, water-resistant, non-fragile, etc.). Despite efforts of scientists, traditional natural materials (wood, leather, metals) may be hard to replace, and there will be a necessity to incorporate these materials.
ORGAN PRINTING
According to Mikolajewska et al, 2014, 3D printing is useful in reconstructive surgery – it allows to reproduce/regenerate the exact nature of affected internal anatomy, eliminate
potential errors, and decrease theatre/recovery time. Reconstruction of the internal anatomy is in these cases based on Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). According to Brandon Griggs (2014), 3D printing will be extremely beneficial to medical students. The manufactured organs will be a perfect representation of organs making learning easier as students will be able to see exactly what a organ should look like (Griggs, 2014). He goes onto saying that these manufactured organs will be better to use in comparison to cadavers. In my opinion i don’t think that this is practical, as diseased human beings organs don’t look perfect; and learning on these perfectly manufactured cadavers does not give students the opportunity to see what a normal humans organs look like. These 3D cadavers will however be beneficial when trying to compare what a normal healthy organ and body looks like in a comparison to a diseased organ or body. These cadavers will also be beneficial when try to illustrate the progression of diseases and the clinical representation of the different types of diseases. This can be done by printing a copy of a type of diseased organs for academic purposes.
ORGAN TRANSPLANTS
The life expectancy of 3D human organs are questionable. The uncertainty of the life expectancy of these organs means that once the life expectancy of the organ is finished and another one needs to be manufactured. This means that another operation needs to be done increasing the risks of postoperative complications of patients.
PROSTHETICS
“Prototyping is useful tool for surgical planning and fabrication of prostheses and implants, including rapid prototyped biomaterials for tissue engineering applications. Current technologies include customised foot orthoses, computer aided prostheses and orthoses development.” (Mikolajewska et al, 2014)
Much of the impact of 3D printing is being seen at present in prosthetics, as it offers a way of providing amputees in countries such as South Sudan and Uganda with prosthetics where this would not have been possible previously due to cost and/or location.
Due to the technology mostly using plastics at the moment the main impact of 3D printing is in the area of upper limb prosthetics. There is another area where the technology may have implications in the UK and that is with the making of the socket. It is the socket fit which is the most vital part of the process and quite often the most time-consuming.
In Uganda the University of Toronto are currently using scanning technology together with 3D printers to help local amputees. After having a scan done of the patient’s residual limb the information is sent to a skilled prosthetist back in Canada who designs the new socket, which can then be printed on the Ugandan machine.
With just 50k skilled prosthetists in the world there are some big gaps to fill though and 3D printers may enable Third World and remote countries to benefit from the work of skilled prosthetists even though they are based thousands of miles away.
SPLINTS
The 3D printed splints are not only more comfortable and attractive but potentially cheaper than the current ones that are ‘ugly, bulky, and can make a patient’s arm sweat’. As a result patients do not use them as often as they should. The splints are made by scanning a patient’s arm in the ‘appropriate position’. A 3D model splint is then designed based on the scan to generate a computer model. The 3D printer can then produce as many splints as are needed at the touch of a button. They can be any colour, feature multiple materials, have a lattice design to aid ventilation and any type of fastening the patient requires.
The Human Rights Acts protects patients from inhuman treatment. Inhuman treatment is quite simply inhuman treatment or punishment which includes: Failing to give medical treatment or taking it away from a person with a serious illness. Medical treatment must never be limited or restricted in anyway. According to the right to life, the human rights act requires the government to protect human life. This means that nobody – including the government – can try to end your life. It also means that you have the right to be protected if your life is at risk. Similarly, public authorities should consider your right to life when making decisions that might put you in danger or which affect your life expectancy.
IMPLICATIONS FOR PHYSIOTHERAPY
According to Mikolajewska et al, 2014, many advances in rehabilitation and physiotherapy have been achieved as a result of advances in other fields.This makes rehabilitation and physiotherapy open to novel approaches and technologies, which can increase effectivity of the therapeutic interventions. 3D printing, can constitute another step toward better application of the rehabilitation engineering principles in current clinical practice.
Weight-bearing joints for the knees, hips and shoulders could be 3D-printed. This means that when a joint is unable to weight bear normally it can be replaced. These joints can be made to accommodate specific weight experienced at the joint. Patient trauma, recovery time and physiotherapy needs would be reduced. This implies that 3D printing will be highly beneficial for patients and it will reduce the rehabilitation period of the patients resulting in the physiotherapists having less work meaning reduction in income for the physiotherapist. According to Mikolajewska et al, 2014, the use of 3D printing in surgical management and strategy of rehabilitation therapy of acetabular fracture makes accurate and safer surgical management of acetabular fracture, shortens postoperative recovery time, promotes postoperative recovery of the patient, and significantly decreases costs.
ETHICAL IMPLICATIONS
It may be easier to approach the ethics of bioprinting by producing regulations and having them voted upon. 3D printing’s ability to manufacture highly customised human organs and anatomical parts will raise inevitable ethical and moral dilemmas, said Pete Basiliere, research director at Gartner. “Saving lives tends to trump all objectives” -Griggs (2014). In this statement Griggs is saying that the main purpose of 3D printing to save lives. Taking into consideration that 3D printing is extremely expensive (Griggs, 2014) and that not everybody will be able to afford it, it makes saving a poorer person’s life highly unlikely (as they can not afford it and the state will most likely not fund it). 3D printing will be bridging the gap between the rich and the poor even bigger (Griggs, 2014).
What happens when complex ‘enhanced’ organs involving nonhuman cells are ,added? Who will control the ability to produce them? Who will be in control of the quality of the resulting organs? Human error will come into play here, making 3D printing less safe and reliable.
Bioprinting is a modern wonder that is fraught with ethical dilemmas. While utilizing such procedures could eliminate the need to animal testing in pharmaceutical trials, it could also lead to a dystopian immortality in individuals that can afford to have organs repaired or replaced as they wear out (Wolinsky, 2014). While some may see this attainable immortality as a blessing, it does raise further concerns. Social justice is a relevant concern in this matter as most likely, money would decide who lives and dies (Wolinsky, 2014). Furthermore bioprinting could become related to performance enhancement in professional sports by becoming a tool to repair injured tissues from playing or training or by unnaturally advancing human capabilities (Wolinsky, 2014). A bioprinted organ black market may result and replace the human organ thieves and black market bidding for donated organs. If unregulated parties are bioprinting organs to make a profit, who is to say that the organs meet quality control standards? (Wolinsky, 2014) Regulation of the organs is a multi-faceted concern. From the medical insurance perspective, would bioprinted organs or mini-tissues be considered a preventive measure or a treatment (Wolinsky, 2014)? Which costly procedures would warrant coverage by a person’s insurance? Furthermore, while copyright laws are a concern with all 3D printing, various medical professionals would benefit from a knowledge sharing networks, but should still credit and reward those who create new codes for bioprinting constructs. On a more ominous note, knowledge sharing of bioprinting practices could also be weaponized for bioterrorism by using malignant or contagious self-replicating organisms (Wolinsky, 2014). In summary, while 3D printing is a paradigm-shifting double-edged sword, bioprinting is an even more complex and possibly dangerous aspect of it.
As stated earlier, there are many ethical considerations regarding bioprinting. Utilitarianism strongly supports its use as we could improve quality of life, cure disease, and repair injury in many individuals by printing repairs or replacements with their own tissues. This also has the potential to reduce or eliminate the use of animal testing in pharmaceutical labs and product testing facilities for the benefit of many species. Duty or deontological ethics, however, creates an ethical dilemma as the rules we have are not yet expansive enough to cover the many ethical concerns regarding bioprinting. For instance, while we have rules regarding who receives organ donations and placement on waitlists, this is because organs must be donated. What happens if new organs can be bought and printed in a matter of days from one’s own tissues? How do we regulate placement in the waitlist to use the printers? Do organs need to be paid out of pocket or billed by insurance to begin the ordering and printing process? For what reasons should printing a new organ be allowed? Should we allow those who can pay for it to print organs to maintain their health leading to a sort of immortality? In the entertainment industry, how will bioprinted repairs or replacements be categorized in professional sports, as a drug/doping or a legitimate treatment? Will plastic surgeons be able to bioprint more aesthetically-pleasing versions of a patient’s body to replace damaged, aging or undesirable tissues?
MORAL CONCERNS
In different contexts 3D printing will seem more appropriate to use than in other contexts. In following statement by Griggs (2014) is of those: “Authentic printed organs should be used for drug or vaccine testing, freeing researchers from less accurate methods such as animal or synthetic models”. In this case no human creature (humans and animals included) will be compromised for medical research and medical advancement.
For religious folks, there is already a dichotomy between determinism and free will,but that is usually presented in the context of behaviour and actions and biology that is when a person dies and it was determined that God decided it was their time. Does that mean any unnatural extensions of life like printing organs from one cells as opposed keeping somebody on life support, which is allowed but temporary extension of natural life not permanent. Extension through a non natural organ are interfering with the deterministic belief. The Catholic church has not made any statement on 3D printing of organs but because religious beliefs often come into contrast with utilitarian beliefs,it’s not entirely certain they will be ok with it.
Ethically and morally concerns have been raised over ensuring the quality of the organs and who controls the right to produce them. Others claim 3D printing human components further blurs the line between man and machine giving us the right to play God on an unprecedented scale. But there is no denying that bioprinting has the potential to revolutionise medicine and health care beyond what seemed possible even 20 years ago.
SUGGESTIONS
As mentioned in physiotherapy implications it is stated that there are benefits to 3D printing for physiotherapy. “With regards to prosthesis 3D printing can provide an inexpensive alternative with greater functionality” (Asher, 2015). That means that physiotherapists and patients will benefit greatly for example patients in rural areas might not have to wait as long as they currently do for a prosthesis IF there is a 3D printer available in that area.
Another example is the 3D printing of splints. With regards to splinting and the 3D printings ability to print splints. It will be convenient for the therapist and the patient as it will be made more accurate to fit the patient perfectly. 3D printing will be very beneficial for our profession allowing us to explore new interventions in treatment. It could possibly quicken recovery time after surgery such as fractures. 3D printers will be able to print replacement parts strong enough to accommodate body weight and weight bearing will not have to take as long, as patients will be able to weight bear immediately.
As beneficial as it may be there are also things that 3D printing will take away from our profession. But ultimately it will add more then what will take away from our profession. It will add more value than do harm.
References
- Anderson, T. (2014). [Online]. 3D Organ Printing. Retrieved September 3, 2015:
- Asher, M. (2015) Printable prosthetics for children. Retrieved from http://www.anatomy-physiotherapy.com/component/content/article?id=1169:printable-prosthetics-for-children
- Coasting Together (2014, January 24) 3D Printing- The future for prosthetics. Retrieved from https://coastingtogether.wordpress.com/2014/01/24/3d-printing-the-future-for-prosthetics/.
- Loughborough University (2014, July 07) Research on 3-D printed wrist splints boost for arthritis sufferers. Retrieved from http://phys.org/news/2014-07-d-wrist-splints-boost-arthritis.html.
- Mikolajewska, E., Macko, M., Ziarnecki, L., Stańczak, S., Kawalec, P.,& Mikolajewska, D. (2014). 3D printing technologies in rehabilitation engineering. Journal of health sciences. 4(12),78-83.
- Mirovon, V., Kasyanov, V., Drake, C., & Markwald, R. (2008). Organ printing: promises and challenges. Regen. Med. 3(1), 93-103.
- Gilpin, L. (2014). [Online]. The dark side of 3D printing: 10 things to watch. Retrieved September 3, 2015: http://www.techrepublic.com/article/the-dark-side-of-3d-printing-10-things-to-watch/.
- Griggs, B. (2015, April 5). The next frontier in 3-D printing: Human organs – CNN.com. Retrieved from http://edition.cnn.com/2014/04/03/tech/innovation/3-d-printing-human-organs/.
- Neely, E.L. (2014). [Online]. The Risks of Revolution: Ethical Dilemmas in 3D Printing. Retrieved September 3, 2015: http://www.academia.edu/8209419/The_Risks_of_Revolution_Ethical_Dilemmas_in_3D_Printing.
- The Human Rights Act. (2015). [Online]. Retrieved September 3, 2015: http://www.equalityhumanrights.com/your-rights/human-rights/what-are-human-rights/human-rights-act.